One of the reason that cancer can be a serious disease is its ability to spread to other parts of the body beyond the location of the primary tumour. When cancer cells spread to distant lymph nodes, tissues or organs, it is called metastatic cancer
LIVER METASTASES ARE CRITICAL
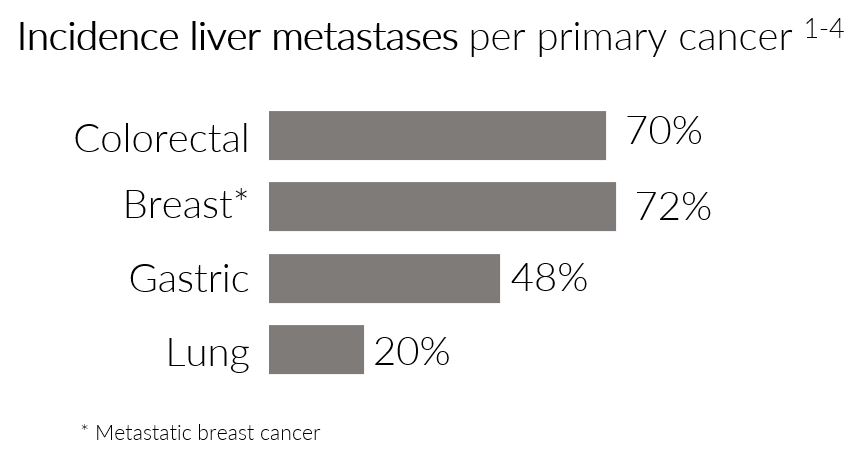
The liver is the second most common organ for metastasis after the lymph nodes. Up to 50-70% of patients with colorectal cancer develop liver metastases, and liver metastases seem to play a significant role in the cause of death of patients who die with breast or colorectal cancer.
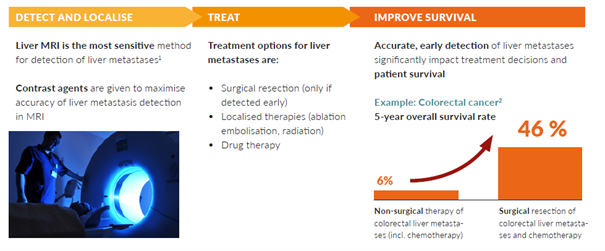
The earlier metastases are detected, the better the chances for successful medical intervention, and ultimately patient survival.
DETECTION AND VISUALIZATION ARE CRITICAL FOR THE MANAGEMENT OF LIVER METASTASES
Correct and early diagnosis is essential for the management of patients with liver metastases. Non-invasive imaging plays an important role in initial diagnosis, pre-operative planning, monitoring of treatment effect, and in surveillance for disease recurrence.
If liver metastases are accurately detected, and deemed eligible for surgical removal, the prognosis can be improved and full recovery is sometimes possible.
MRI IS THE RECOMMENDED IMAGING MODALITY
Magnetic Resonance Imaging (MRI) enhanced with a contrast agent is considered the preferred and most sensitive imaging modality for clinical non-invasive assessment of liver metastases and primary liver cancer.
This imaging method uses radio waves and strong magnets to create valuable di¬agnostic images. Unlike CT and PET-CT, these images are made without exposing the patient to radiation.
CONTRAST AGENTS IMPROVE MRI-SCANS
Patients are given contrast agents prior to MRI scans to enhance the imaging quality. A contrast agent is a substance that makes abnormalities, such as metastases, appear clearer.
This is due to the special magnetic properties of the elements in the contrast agent, which aim to increase the sensitivity and specificity of the image compared to an MRI without the use of a contrast agent.
Currently available MRI contrast agents are based on the toxic heavy metal gadolinium.
- Fowler et. al, Ann Surg Oncol, 2013, 20:1185–1193.
- Clinical Colorectal Cancer, Vol. 15, No. 4, Dec 2016, e183-192
CONTRAST AGENTS CURRENTLY ON THE MARKET ARE NOT FOR EVERYONE – ORVIGLANCE® AIMS TO FILL THIS GAP
Patients with severely impaired kidney function, who are exposed to the gadolinium used in currently available contrast agents, are at risk of the serious and potentially fatal condition Nephrogenic Systemic Fibrosis (NSF).
NSF is a rare, but serious and life-threatening condition that causes extensive waxy thickening and hardening of the skin. It can lead to joint contractures and muscle and fascial fibrosis, which may lead to severe immobility. It can also affect the inner organs. NSF worsens over time and can cause death, which typically results from multi-system failure due to sclerotic transformation of organ systems.
Regulatory agencies, including the FDA and EMA, have released warnings about the use of GBCAs and clinical guidelines provide restrictions for the use in patients with severe kidney impairment. Therefore, all gadolinium-based contrast agents (GBCAs) have black box warnings in their label for this patient population.
Today, the standard management of patients with severely impaired kidney function is liver MRI without a contrast agent; also called an unenhanced MRI. However, this reduces the ability to detect and visualize, and therefore optimally treat liver metastases. An unenhanced MRI consequently risks reducing patients’ chances of survival.
There is, therefore, a need for a safer liver contrast agent for patients with severely impaired kidney function. Orviglance* aims to fill this role and be the standard of care for this patient population.
Please note that Orviglance is an investigational medicinal product and is not yet approved for use by regulatory authorities in any jurisdiction.
*Trademark is registered in Europe and several other markets and submitted for registration in the US.
References for the first graph:
- Riihimäki, M. et al. Patterns of metastasis in colon and rectal cancer. Sci. Rep. 6, 29765; doi: 10.1038/srep29765 (2016); Journal of Pathology, 2014, 232:23-31
- Oncotarget, 2016, 7(32):52307; Lung Cancer, 2014, 86:78-84 (6):29765
- Guy diSibio and Samuel W. French (2008) Metastatic Patterns of Cancers: Results From a Large Autopsy Study. Archives of Pathology & Laboratory Medicine: June 2008, Vol. 132, No. 6, pp. 931-939
- Rahbari et al. Metastatic Spread Emerging From Liver Metastases of Colorectal Cancer: Does the Seed Leave the Soil Again? Annals of Surgery: February 2016 – Volume 263 – Issue 2 – p 345–352